Box-checking and deadlines are important, but are they "Science"?
If there was any doubt whether I’m middle-aged, I am, in fact, past middle age, as I will turn 40 in December. The average life expectancy for a 39-year-old male in the United States is 37.85 years per the Social Security Administration actuary tables. the kids started school last month and it has been one back-in-my-day moment after another ever since.
This is the most recent one: the eldest has started 6th grade, which in the US is considered Middle School, and is apparently a big deal because that is when they start getting actual grades. Now, back in my day and — this is probably the more relevant fact — in Serbia, you started getting properly graded scored
The unfortunate characteristic of the American school system is that it uses the term “grade” for too many distinct but adjacent concepts, so I will stick to “grade” for the yearly cohort of kids, and use “score” for the number they get on assignments and at the end of each year. in 1st grade: there was none of this descriptive assessment shenanigans. It was also probably the reason why the teachers were so interested in what your parents did for a living. But this is not a tirade against descriptive scoring; I had that moment 5 years ago at our first encounter with the 1st grade. The 6th grade b-i-m-d moment was that the scoring is performed nearly real-time, is viewable by both parents and children via an online portal, and — this is what got me — includes whether you:
- wrote your full name instead of only the first name on a line that says just “Name”;
- checked all of the boxes on an end-of-class exit form, regardless of whether you performed the tasks outlined next to those boxes;
- turned in your field trip forms on time.
This is all incorporated into your Science class score. Science. Class. Score.
Now, if the main goal in your life as a scientist is to apply to as many NIH grants as possible and perhaps even win some of them, then yes, science is mostly about box-checking and meeting deadlines. But if you want to call these endeavors “science”, I encourage you to scroll through Adam Mastroianni’s newsletter Experimental History and check your beliefs against some persuasive evidence that science is, in fact, the complete opposite of checking boxes and worrying about the next deadline, and that part of the reason it is stagnating (well, some sciences more than others) and that younger generations are more interested in becoming influencers, content creators, crypto millionaires or whatnot is that they have this misshapen idea about what science actually is from the backwards way it is being presented to them.
With good intent, I should add! There absolutely should be a way to encourage tweens, teens, and adolescents to be more responsible and contentious and middle school is as good of an age to start as any. Heck, there is even a ready-made textbook for it. But call it “life skills”, call it “civics”, call it “behavior” if you will, as we did back in my day. Just please don’t call it Science.
Update: if you thought my quip about box-checking skills being important for NIH grants was facetious, here is the winner of the 2021 Nobel Prize for Medicine describing a recent desk rejection from the NIH for failing to properly format his references on a grant application. Quo vadis, scientia?
Things I got wrong: in-person versus online
We are three weeks into our clinical trials course for the UMBC graduate program. This remark will surprise absolutely no one, but: it was refreshing to see a classroom full of attentive, engaged students, interrupting, asking questions, having a dialogue, others jumping in, etc. Alas, I cannot take any credit for the interactions, as we have guest lecturers on for most weeks.
Regardless, the course has reminded me about how absolutely wrong I was back in December 2019, when during a post-conference The link is for the 2019 ASH Annual Meeting abstract book, ASH being the American Society of Hematology, and I am only now realizing that — in what could be described as our profession’s version of burning man, which is actually quite fitting for an organization called ASH — they tear down the conference website each year to make a new one. So, the 2019 version is no more, but here is one for the 65th annual meeting in December 2023 although if you go to the website after December 2023 I am sure it will point you to the 66th and beyond. I could have linked to the Internet Archive version of the website from 2019 instead — in fact, here you go — but why relinquish myself of the opportunity for that burning man’s ash pun? dinner I stood on my soapbox and wondered in amazing why we were still wasting our time meeting in person once per year like barbarians, when we could in fact be having continuous virtual conversations on Zoom. Timely spread of scientific information and all that.
Well, I have apologized — in person! — to everyone who had to suffer through my Orlando diatribe, because the last 3 years have shown that while video conferencing may rightfully replace most business calls and other transactional meetings, it is absolutely abysmal for education for all parties involved. And it’s not just that any kind of non-verbal communication is lost, it is that even spoken language is stilted, muted, suppressed. With the slide-up-front, speaker-in-the-corner layout that is so common for lectures, you may as well be pre-recording it. It makes absolutely no difference.
And, attending a few online lectures every month myself, it is hard to decide what is worse: having it be completely online and trading off the quality of the lecture for more opportunity for interaction, or watching a live/hybrid lecture and being completely shut out from the discussion (because the in-person attendees take priority when it comes time to ask questions, and rightfully so).
Even at the most basic practical level: technology failure with an online lecture means no lecture; technology failure in-person means, at worst, using the whiteboard and interacting more, which actually makes me wish for more technology to fail. And if you absolutely need to have the slides to make your points, just print them out for your own reference, and share them beforehand for the students to view on their own screens, of which they will have many.
Craig Mod had similar thoughts this week about work in general:
After the last couple of weeks of in-person work, I have to say: Some things simply can’t be done as efficiently — or at all — unless done in person. The bandwidth of, and fidelity of, being in the same room — even, maybe especially, during breaks and downtime, but during work periods, too, of course — of being able to pass objects back and forth, to have zero latency in conversation between multiple people. To not fuss with connections or broken software (Zoom, a scourge of computing, abjectly terrible software (I prefer … Google Meet (!) by a mile)) or cameras that don’t allow for true eye contact — where everyone’s gaze is broken and off and distracted. To dispatch with all of those jittery half-measures of remote collaboration and swim in the warm waters of in-person mind-melding is a privilege for sure, and a gift.
Education is one of those types of work that can not easily be replicated online. AR/VR being a big and obvious caveat here, but that will take a while. For evidence, look no further than the persistence of the physical university campus despite the plethora of free and paid online options. Were it not for the in-person factor, the higher education equivalent of The New York Times would have gobbled up the market by now. I’ll know the tide has turned once Harvard and Yale — which would be my first proxies for the NYT and WaPo of higher ed — start investing more in their online offerings to the detriment of in-person experience.
Kudos to the two physicists who plotted all objects in the Universe onto a single 2D plot, most of all for the breadth of their ambition, but also for planting their tongue firmly in cheek with a tiny, sub-Planckian-sized quip:
Humans are represented by a mass of 70 kg and a radius of 50 cm (we assume sphericity), while whales are represented by a mass of 10^5 kg and a radius of 7m.
Someone please update Wikipedia! (ᔥJason Kottke)
Target-based drug discovery is a waste of time, says a systematic review of 32,000 articles and patents from the last 150 years:
…only 9.4% of small-molecule drugs have been discovered through “target-based” assays. Moreover, the therapeutic effects of even this minimal share cannot be solely attributed and reduced to their purported targets, as they depend on numerous off-target mechanisms unconsciously incorporated by phenotypic observations. The data suggest that reductionist target-based drug discovery may be a cause of the productivity crisis in drug discovery.
So it would seem. And even those drugs initially developed to target a single protein or mutation end up having many more unanticipated effects. Back to the jungle and the ocean depths, then?
(ᔥDerek Lowe)
As a prolific child fabulist, I very much appreciated @ayjay’s reminiscence. Most people are, in fact, reflexive embellishers, but not everyone can recognize it in themselves or turn it into a healthy skepticism. At least that’s what I tell myself!
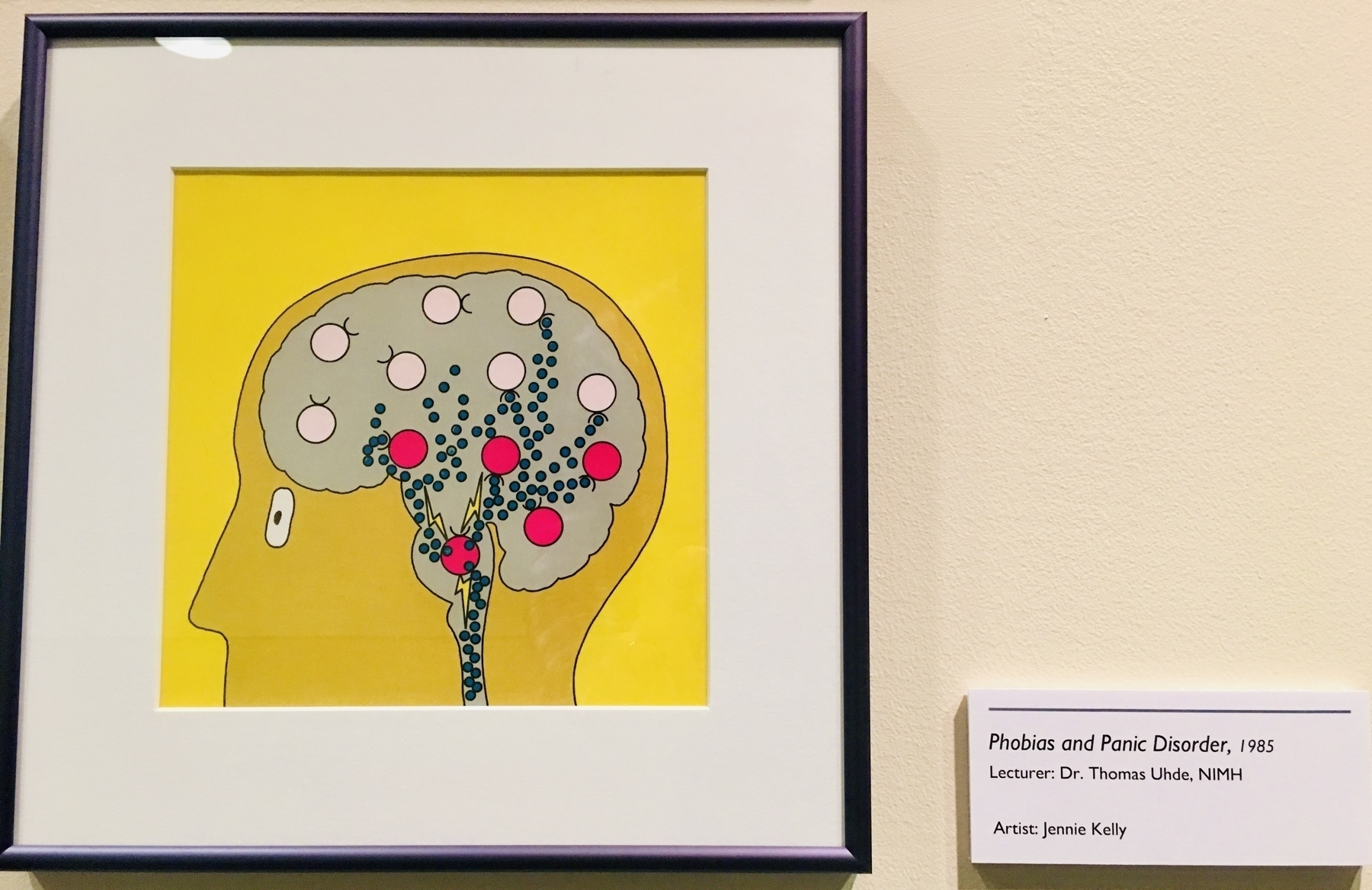
The NIH Clinical Center used to commission artwork for some of their lectures. Here is one for “Phobias and Panic Disorder” from 1985.
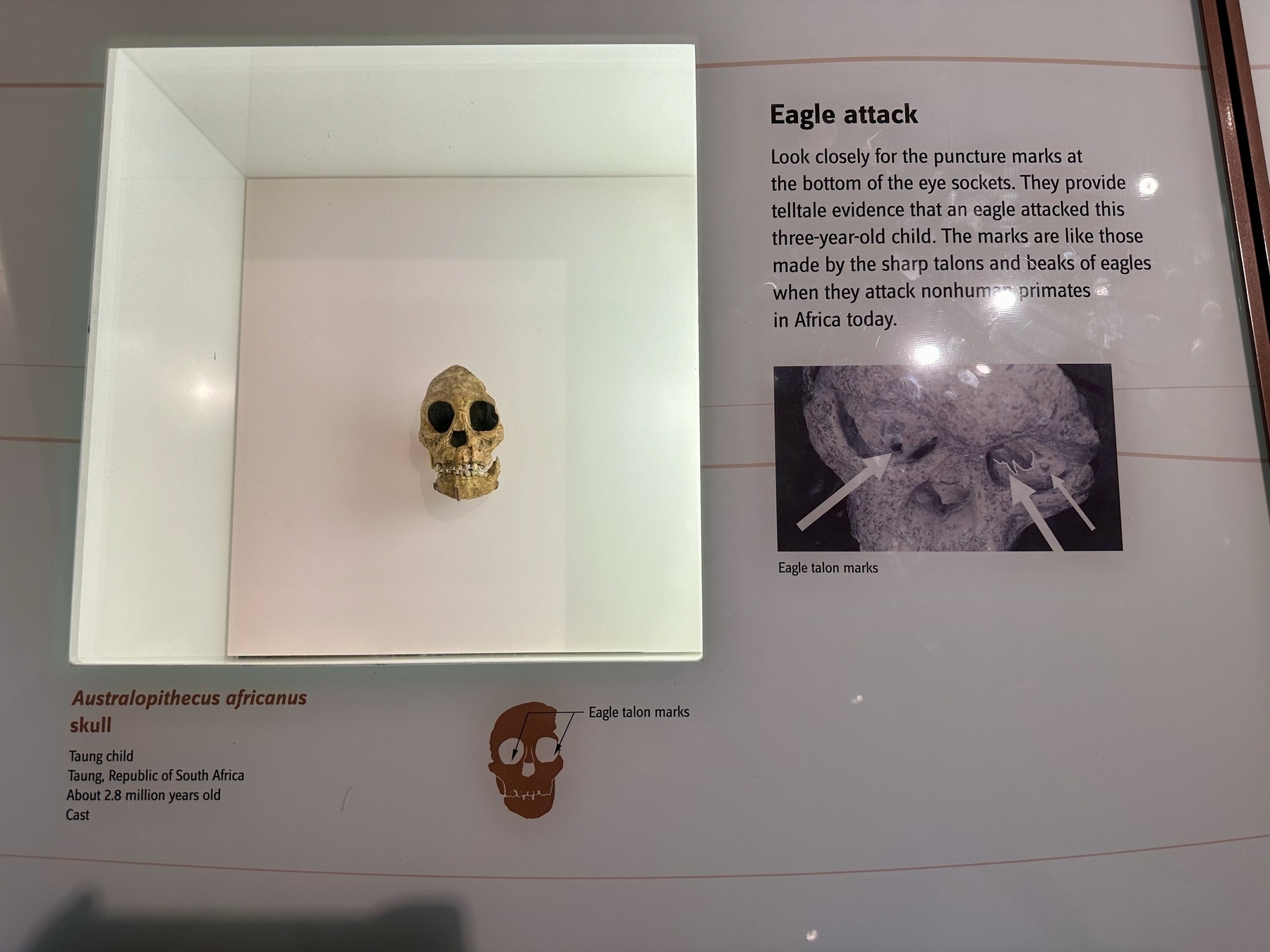
In retrospect, that friend worried about an eagle flying away with his toddler as prey wasn’t completely bonkers.
From the early humans exhibit at the National Museum of Natural History.
Derek Lowe writes about a recent Cancer Cell paper pitting glioblastoma cells against each other in a mouse model:
A single clonal line that hit on high Myc expression could outcompete fifteen thousand others from a standing start!
As someone who’s treated patients with Burkitt lymphoma, the Myc-dependent cancer, I can absolutely believe this.
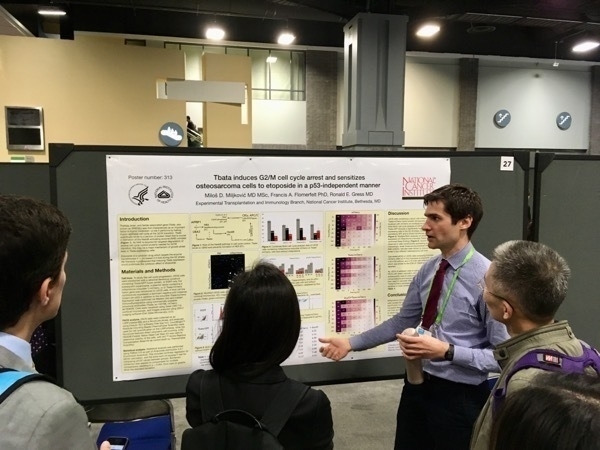
From the archive: the author presenting some preclinical work on the cell cycle at the AACR annual meeting in Washington DC, circa 2017. Little did I know that six years later I’d be living just a few blocks down the street.
More crowded than usual.
For your (and mine, time permitting) weekend reading, listening, and/or viewing pleasure: the Tim Ferris interview with Nassim Taleb and Scott Patterson. I sure hope you are familiar with the former; the latter is a reporter for The Wall Street Journal who also wrote a book about “black swan traders”, which, yes, is probably going to the pile the antilibrary. It is a 2-hour discussion rightfully described as a feast.