From the American Journal of Obstetrics and Gynecology:
The high and rising rates of maternal mortality in the United States are a consequence of changes in maternal mortality surveillance, with reliance on the pregnancy checkbox leading to an increase in misclassified maternal deaths. Identifying maternal deaths by requiring mention of pregnancy among the multiple causes of death shows lower, stable maternal mortality rates and declines in maternal deaths from direct obstetrical causes.
Translation: maternal mortality often went undetected, so they changed the way we had to measured it. We don’t like how the new way of measuring is making us look compared to other countries, so we want to change it back. Goodhart wins again. (↬Washington Post)
“Maybe that’s why young people make success. They don’t know enough. Because when you know enough it’s obvious that every idea that you have is no good.”
This was Richard Feynman per the James Gleick biography, and he was correct! Biomedicine is now in this position, as I wrote yesterday.
The low-hanging fruit of medicine
The Medical Journal of Record The New York Times. The link is to a gift article. has an excellent story on Kawasaki disease out today which reminded me of Balkan endemic nephropathy, another rare disease with an unusual and infectious disease-like distribution. Note that prevalence and distribution are where the similarities end. Kawasaki disease is a vasculitis (inflammation of the blood vessels) that affects children and young adults. Balkan endemic nephropathy caused your kidneys to shrivel up and stop working, and affected the middle-aged and the elderly. It had no known cause back when I was in medical school (which was — gasp — 20 years ago), but it has since been tied to accidental consumption of a certain plant. Well, accidental in the Balkans but intentional in China, where it was used in some traditional medicines and could cause “Chinese herbs nephropathy”, which was like the Balkan version on speed. Note that I am referring to both BEN and CHN in the past tense, but should probably temper my enthusiasm: even though we know what’s causing them and how to prevent them, their prevalence has decreased but is not zero.
The genetic revolution has been great for many aspects of medicine, but it has also made us a bit lazy. The promise of the late 1990s and the early 2000s has been that we would fine the genetic cause of most diseases, and would be only a step away from solving them. While we certainly found many genetic disorders, most of the are in the ultra-rare category and tied to newly-established diseases that were previously only described as syndromes. The “big” diseases — hypertension, type 2 diabetes mellitus, major depression and the like — are as unknown as ever, their cause described as “multifactorial” which is code for “we don’t know”. Stomach ulcers were also thought to be multifactorial until we found out they were mostly caused by a bacterium. A similar thing seem to be happening with multiple sclerosis, which seems to be caused by a virus, one that was mostly thought to be an unavoidable nuisance but is now a vaccine target.
But haven’t we already discovered all the big bad bugs? I sincerely doubt it. We have trouble identifying even larger organisms Also a gift link, this time to The Washington Post. I’m on a roll today. — there could be hundreds of disease-causing creatures and substances that we don’t yet know about because we can’t see them, can’t grow them, and/or don’t know where to look. And we terrifyingly bad at looking for anything but the obvious — there are parts of our own anatomy that we’ve discovered just recently.
So, I know that we will find the cause of Kawasaki disease and can only hope that it will be soon. I also hope that we will find the one main cause of the obesity epidemic. Add in essential hypertension and psychiatric disorders in there. Much money has been spent on discovering the genetic factors of these diseases. Now that we know that genes play but a small part in most of them, maybe it’s time to reallocate the funds.
Alex Tabarrok gives name to something we’ve all experienced:
Ironically, just as measles can induce immunological amnesia, vaccines can induce social amnesia about the severity of diseases, thereby making society more susceptible to pathogens that they previously were able to resist.
“Vaccine-induced social amnesia” is a good way to describe it. See also: people who ex post claim we never needed covid-19 lockdowns when the truth is in fact the opposite.
I wish King Charles the best in light of his cancer diagnosis. Reading some of the old coverage of his health issues I noticed that both of his parents had “old age” listed as the cause of death. Any certifying MD that tried to pull that over here would have had the paperwork returned in an instant.
February lectures of note
- Demystifying Medicine — Hepatitis D and E: New Challenges and Progress by Drs Theo Heller and Marc Ghany (NIDDK), Tuesday February 13 at 4pm EST
- How Memory Meets Perception During Naturalistic Scene Understanding by Dr Caroline Robertson (Dartmouth College), Wednesday February 14 at 1pm EST
- Demystifying Medicine — Sickle Cell Anemia: a Global Perspective by Drs Ambroise Wonkam (JHU) and Courtney Fitzhugh (NHLBI), Tuesday February 20 at 4pm EST
- WALS Lecture: Tale of Two Cities: Disease Based Research or Geroscience? by Laura Niedernhofer (University of Minnesota), Wednesday February 21 at 2pm EST
- Demystifying Medicine — Global Warming and Human Adaptation by Drs Gabriel Vecchi (Princeton) and Michael Sawka (Georgia Tech), Tuesday February 27 at 4pm EST
- Diversity in Clinical Trials: The Barriers and the Opportunities by Dr Youssef Roman (FDA), Wednesday February 28 at 12pm EST
- Influenza Pathogenesis and Therapeutics in Vulnerable Populations by Dr Stacey Schultz-Cherry (St Jude), Wednesday February 28 at 2pm EST
The wellness visit
I am not a fan of “wellness” visits, those yearly exams that your insurance insists you should do even if you don’t have any medical problems. Evidence from randomized controlled trials suggests they don’t make any difference to people’s health, but they (obviously) contribute to the primary care physicians' workload.
Having said that, I recently reached a nice round number of years, so it was time to get my cholesterol checked and finally get a flu shot. I enjoyed the banter, but I could also see how and why there may be no health benefit. If annual exams are good for anything, it is to find chronic asymptomatic conditions that have long-term consequences — high blood pressure, high cholesterol and high glucose are the big ones at my age. Testing for them has the highest yield in a generally low-yield visit, so whoever is seeing you should get at least those three right.
After this morning I suspect most places are not doing it right. The person checking my blood pressure did not care at all about the correct technique: whether I still had my sleeves on when they placed the cuff, whether my feet were on the ground or hanging over the raised exam table, whether my legs were crossed, or whether I was talking while measurement was being taken. Worse yet, no one asked or cared whether I had anything to eat or drink before getting my blood drawn for the labs. I could have downed a sugar-and-cream-laden coffee with a Boston cream chaser minutes before the visit and no one would have known. This is the complete opposite of Serbia, where they drill into you at an early age that you must have nothing to eat or drink — water excepted — before getting your blood drawn for anything; which is an extreme of its own kind but one that at least doesn’t result in lab results that you can’t interpret.
At best the loose approach to testing leads to more labs having to be drawn if and when something comes back out of range and the doctor wonders why. At worst it leads to misdiagnosis (“Your cholesterol is through the roof, you’d better be on a statin!") or missed diagnosis (“Your cholesterol is a bit too high but you ate before the labs were drawn so it’s probably just from the food.") — neither is good.
Even when properly done, I don’t think the annual exams are worth it. There are plenty of reasons to see the physician for other things, and sneaking in a blood pressure check and some labs on top of those is easy enough without overburdening the system. For those fortunate enough to be without ailments, a visit every 5–10 years to make sure all the screenings are up to date sounds about right. The paradigm of treating your body as a car to be taken to the shop for scheduled maintenance is wrong: our bodies aren’t intelligently designed mechanisms with replaceable parts that wear out at a predictable rate, and we can’t be taken apart and put back together at a whim. The trend of renaming the annual exam to something else recognizes this reality.
The replacement term, wellness visit, is not much better. In theory it should make the doctor (or nurse practitioner) enhance the lives of people they are seeing by taking a more holistic approach: “You are not a patient, you are a person.” In practice, it turns doctors into box-checkers: are you suicidal (yes/no), do you drink alcohol (yes/no), do you use illicit drugs (yes/no). It takes time away from things doctors were trained for — to treat disease that can be treated, provide council about the diseases that can’t, and know the difference between the two — and makes them do things that are as important, maybe more so, but not in their area of expertise.
The problem isn’t unique to medicine. It’s good to have the police around to deal with murder and theft, not so much when there is a domestic dispute or an acute psychotic episode, now (holistically?) called “a mental health crisis”. They used to be matters for the extended family or neighbors to deal with, not an outside force. Wherever the two were lost, public and private services picked up some of the responsibilities; the doctors seem to have gotten the role of the friendly ear, listening to the issues that used to be mulled over a cup of tea, or — sure, I’ll go there — in the bowling alley. This is a job they were not trained to do and for which they receive no compensation, so in that sense it is fair: the (American) society got what it paid for.
Theory and practice, drug cost edition
You know the one about theory and practice? That in theory there is no difference between the two, but in practice there is. Yesterday’s post from the economist Alex Tabarrok about better drugs costing more is a great example. Per Tabarrok:
Consider two lightbulbs, one lasts for 2 years the other lasts for 1 year. Which lightbulb is more profitable to sell? Any sensible analysis must begin with the following simple point: A lightbulb that lasts for 2 years is worth about twice as much as a lightbulb that lasts one year. Thus, assuming for the moment that costs of production are negligible, there is no secret profit to be had from selling two 1-year lightbulbs compared to selling one 2-year lightbulb. The firm that sells 1-year lightbulbs hasn’t hit on a secret profit-sauce because its customers must come back for more. If it did it could sell really profitable 1-month bulbs!
The same thing is true for pharmaceuticals. A treatment that lasts for 10 years is worth about ten times as much as an annual treatment. Or, to put it the other way, a treatment that lasts for 10 years is worth about the same as 10 annual treatments producing the same result. (n.b. yes, discounting, but discounting by both consumers and firms means that nothing fundamental changes.)
Too bad that drugs aren’t lightbulbs, hospitals aren’t hardware stores, and that treating people isn’t the same as selling tchotchkes. Well, maybe they are the same in theory, but we looked at actual cancer drugs, and their actual cost, and how much the cost per year correlates with actual improvements in survival, and the answer was: not at all. Novelty of the mechanism of action doesn’t have much to do with the cost either. We didn’t go into what affected the cost, but as I’ve written before, President Biden made a good guess.
So yes, lightbulbs. Cute story, professor Tabarrok, but true only in theory.
Here are Mr. and Mrs. Phillip Wase, as seen at the Smithsonian American Art Museum.

The odd and disengaged looks they both have aside, does Mrs. Wase look like she has a medical condition? Here is a hint.
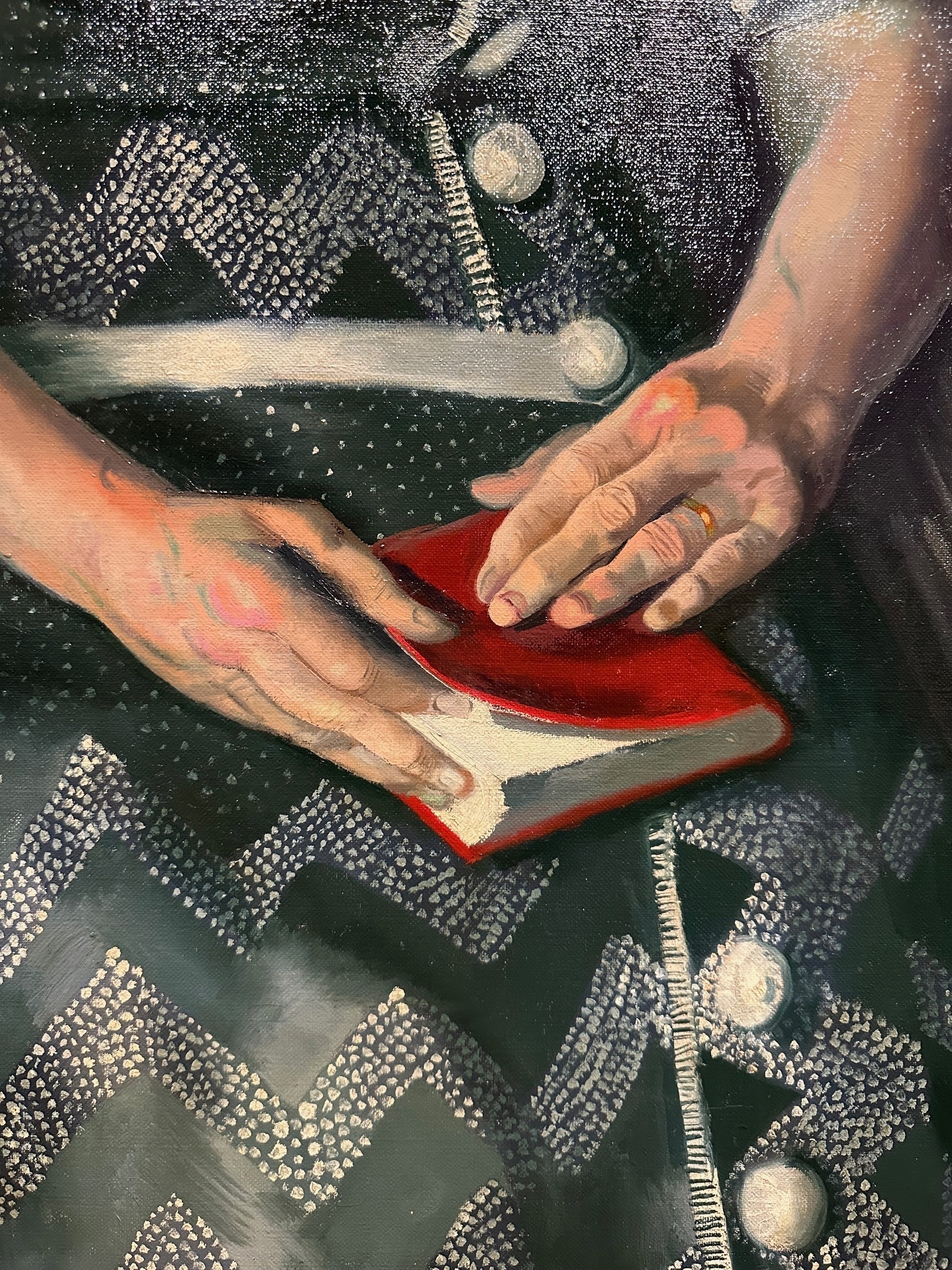
This looks like textbook swan neck deformity, so Mrs. Wase probably had rheumatoid arthritis.
Tim Harford on the UK’s crumbling health care system:
In the case of St Mary’s Hospital in London, these weak foundations are all too literal. The Financial Times recently reported that the hospital had rotting floor joists, frequent flooding, a hole in one lavatory floor that led to a car park, a ward closed due to a collapsed ceiling, and sewage backing up out of the drains and into the outpatient department. Yet St Mary’s is no longer regarded as an urgent priority for investment, because five other hospitals appear to be in more imminent danger of falling down.
15-some years ago, when I was contemplating what to do after graduating from medical school, the UK was on the list of places for potential residency. It quickly got crossed off because it was hostile to foreign doctors — especially compared to the US — but good for me that it was!